Research Article, Arch Transplant Vol: 7 Issue: 1
Collagen Patch Repair of Tympanic Membrane Perforation
MK Rajasekar*, Shwetha Shashikumar, Monica
Department of Otorhinolaryngology (ENT), Sree Balaji Medical College and Hospital, Chennai, Tamilnadu, India
- *Corresponding Author:
- MK Rajasekar
Department of Otorhinolaryngology (ENT),
Sree Balaji Medical College and Hospital,
Chennai,
Tamilnadu,
India,
Tel: 9447590782;
E-mail: shwetha.shashikumar93@gmail.com
Received date: 21 January, 2023, Manuscript No. AT-23-87644; Editor assigned date: 23 January, 2023, PreQC No. AT-23-87644 (PQ); Reviewed date: 06 February, 2023, QC No. AT-23-87644; Revised date: 13 February, 2023, Manuscript No. AT-23-87644 (R); Published date: 22 February, 2023, DOI: 10.4172/AT.1000130
Citation: Rajasekar MK, Shashikumar S, Monica (2023) Collagen Patch Repair of Tympanic Membrane Perforation. Arch Transplant 7:1.
Abstract
The aim of this study was to investigate how fibrinogen based collagen graft repair of central perforation, performed endoscopically improves both hearing and ear discharge. This study was done to see how effective the closure of small tympanic membrane perforations using collagen patch would be. This was performed on 30 patients. This procedure was carried out as an office procedure under local anaesthesia, and all patients had consented to participate in the study after hearing the merits and demerits of fibrinogen based collagen patch closure of tympanic membrane perforations.
Keywords: Fibrinogen; Collagen patch; Tympanic membrane; Perforation
Introduction
One of the most common problems otorhinolaryngologists encounters is the perforation of tympanic membrane, which may result in hearing loss and persistent otorrhoea when left untreated. Many small perforations may heal spontaneously with time, but some tend to persist due to infection.
Over the years, many graft materials have been used with varying success rates. An array for graft materials have been tried some of which are: Temporalis fascia, perichondrium, conchal or tragal cartilage, fat. Xenografts like porcine small intestine submucosa, and biomaterials like paper patch, gelfoam and hyaluronic acid derivatives, and genetically engineered biomaterials like silk fibroin, calcium alginate, chitosan and collagen have also been tried. This study was designed to find out the efficacy of collagen patch technique in order to close small sized perforations of the tympanic membrane [1]. The fibrinogen based collagen consists of a sponge like patch which is composed of equine collagen and is coated with a mixture of human fibrinogen, bovine thrombin, and bovine aprotinin. It adheres strongly to tissue, forming a waterproof membrane [2].
Materials and Methods
• This study was done over a period of one year (June 2019-June 2020) in the ENT department of Sree Balaji medical college and hospital, to see the effectiveness of collagen patch in the closure of small tympanic membrane perforations. History was taken, clinical examination, and preoperative work up was done.
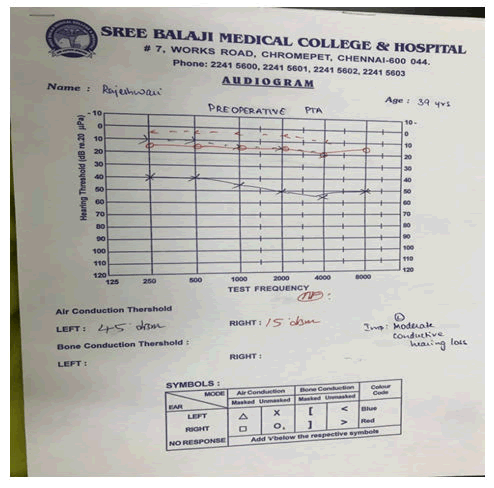
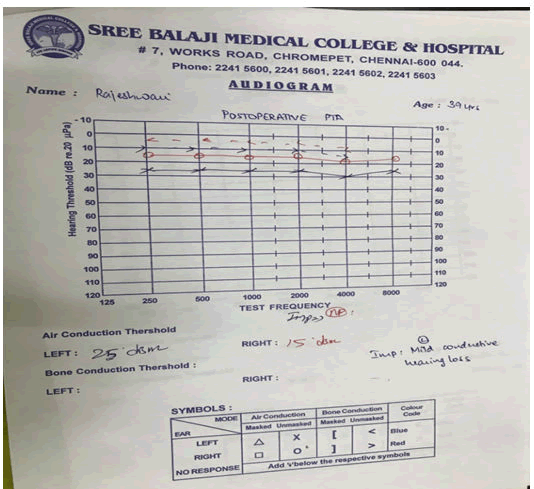
• Pure Tone Audiometry (PTA) was performed both preoperatively and postoperatively. Air-Bone (A-B) gap was estimated at 0.5 kHz, 1 kHz and 2 kHz for all the patients in this study.
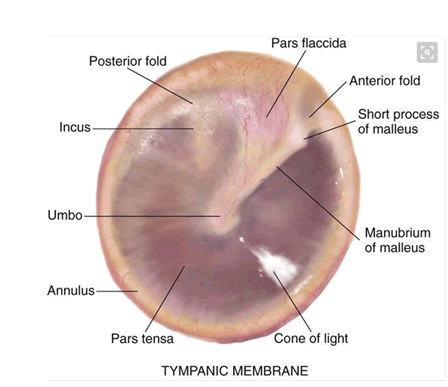
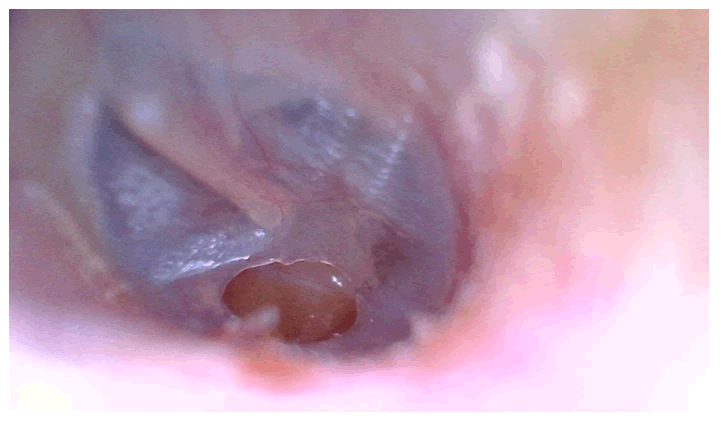
• There were 30 patients who were included in this study, all of whom had consented to participate after hearing the merits and demerits of fibrinogen based collagen patch closure of tympanic membrane perforations (Figures 1 and 2) [3].
Technique
• This procedure was done as an office procedure under local anaesthesia.
• First, 4% Xylocaine solution soaked cotton ball was kept in the external auditory canal.
• Patients were placed in the supine position with the head placed over the head ring and turned to the opposite side of perforation.
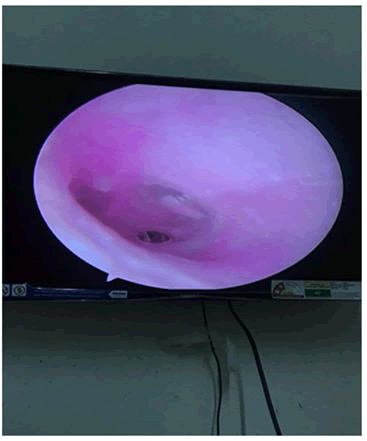
• Under strict aseptic precautions, Hopkins 0° endoscope was used and local anaesthesia was given in EAC using 2% Xylocaine mixed with Adrenaline.
• Margin of perforation was freshened using a sharp dissector.
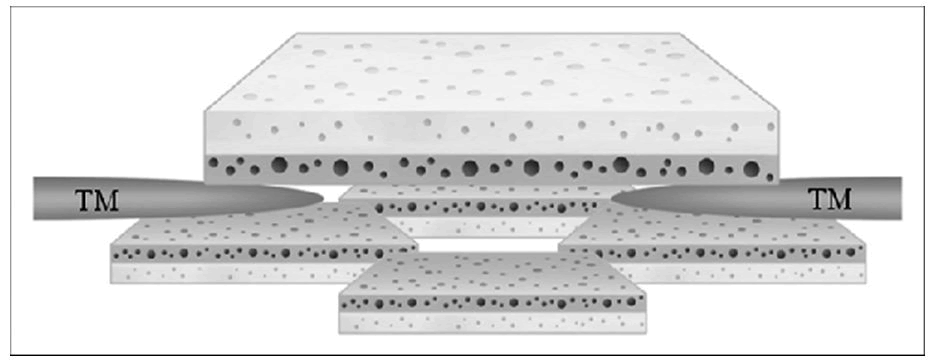
• Collagen sheet was trimmed approximately to twice the size of perforation and placed in sterile saline solution.
• The collagen patch was inserted into perforation, such that it sticks to the overlying surface; to keep it in position and to promote healing, pieces of gelfoam were kept on and around the collagen patch.
• All patients were advised to keep the ear dry, avoid straining or nose blowing for at least 1 month, and to regularly follow up in OPD at the end of 7, 14, 30 and 60 days.
• The appearance of dimeric tympanic membrane was monitored in each follow up.
• Audiometry was done at the end of 1 and 2 months (Figures 3-5) [4].
Results
This procedure has an advantage of least pain and trauma to the ear drum due to the absence of skin incisions, metal flap dissections and fewer complications. Collagen grafts are fully transparent and hence the margins of the perforations can be easily seen by the surgeons. It facilitates monitoring of the postoperative events due to its transparency. An added advantage of this procedure is maximum improvement of the air bone gap after the procedure.
However, it cannot always be an alternative to the conventional surgical myringoplasty. The study consisted of 30 patients, of which 11 were male and 19 were female between the age group 15-50 years. Patients with smaller size perforations were chosen as part of the study. The outcome measures of this study were based on perforation closure, post-operative air bone gap, absence of any complications like infection, persisting defect in the tympanic membrane, collagen patch extrusion or otomycosis (Table 1) [5].
| Gender | Frequency | Percent | Valid percent | Cumulative percent | |
|---|---|---|---|---|---|
| Valid | Female | 19 | 63.3 | 63.3 | 63.3 |
| Male | 11 | 36.7 | 36.7 | 100 | |
| Total | 30 | 100 | 100 | ||
Table 1: Gender distribution.
• Of the study population, 63.3% were female and 36.7% were male.
• Anterior quadrant perforations were found to be more in our study, of which the most common were in antero-inferior quadrant (50%). 10% cases comprised of antero-superior quadrant perforation. Superior quadrant perforation was comparatively less in our study. 6.7% cases comprised of posterosuperior quadrant perforation and posteroinferior quadrant perforations were found in 33.3% cases [6].
• Infective (50%) and traumatic causes (33.3%) of perforation were found at a higher quadrant. Post-myringoplasty cases (16.7%) were found to be less common (Tables 2 and 3).
| Types of tests | Value | df | Asymp. sig. (2-sided) | Exact sig. (2-sided) | Exact sig. (1-sided) |
|---|---|---|---|---|---|
| Pearson chi-square | 30.000a | 2 | 0 | 0 | |
| Likelihood ratio | 36.652 | 2 | 0 | 0 | |
| Fisher's exact test | 29.017 | 0 | |||
| Linear by linear association | 20.471b | 1 | 0 | 0 | 0 |
| N of valid cases | 30 | ||||
| Chi-Square tests | |||||
| Point probability | |||||
| Pearson chi-square | 0.000b | ||||
| Likelihood ratio | |||||
| Fisher's exact test | |||||
| Linear by linear association | |||||
| N of valid cases | |||||
Note: a: 4 cells (66.7%) have expected count less than 5. The minimum expected count is 2.10; b: The standardized statistic is -4.524
Table 2: Chi square tests.
| Type of outcome | Frequency | Percent | Valid percent | Cumulative percent | |
|---|---|---|---|---|---|
| Valid | Healed cp | 7 | 23.3 | 23.3 | 23.3 |
| Complete closure | 14 | 46.7 | 46.7 | 70 | |
| Incomplete closure | 9 | 30 | 30 | 100 | |
| Total | 30 | 100 | 100 | ||
| Outcome | |||||
| Failure | 9 | 30 | 30 | 30 | |
| Success | 21 | 70 | 70 | 100 | |
Table 3: Table showing outcome.
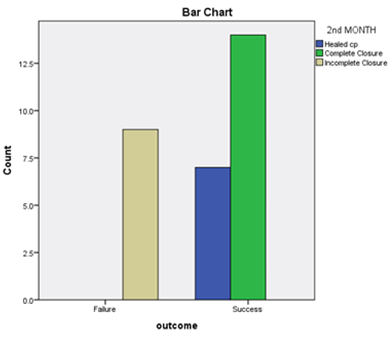
• In our study, collagen patch closure was found to have a success rate of 70% and is a viable graft material for small perforations (Figure 6).
• Traumatic (38.1%) and post-myringoplasty (19%) cases had shown a higher success rate compared to infective group (42.9%).
• Infective causes showed a higher failure rate (66.7%) when compared to other causes (traumatic-22.2%, post myringoplasty-11.1%).
• In our study, 30 % of failure cases were due to collagen extrusion as compared to other causes.
• Audiogram of a patient with 45 dB hearing loss. Two months after collagen patch closure of the perforation a gain of 20dB was noted, indicating improvement in hearing (Table 4, Figures 7 and 8) [7].
| Age | Initial ab gap (dB) | AB gap (Db) 2ndmonth | ||
|---|---|---|---|---|
| N | Valid | 30 | 30 | 30 |
| Missing | 0 | 0 | 0 | |
| Median | 36 | 22 | 14 | |
| Range | 34 | 8 | 10 | |
| Minimum | 16 | 18 | 10 | |
| Maximum | 50 | 26 | 20 | |
| Percentiles | 25 | 26.25 | 20 | 12 |
| 50 | 36 | 22 | 14 | |
| 75 | 42 | 24 | 16 | |
Table 4: Table showing initial and 2nd month ab gap.
While analyzing the collagen patch uptake, and the preoperative and postoperative air bone gap, it was observed that 46.7% of the patients (n=14), showed complete closure of the tympanic membrane perforation following collagen patch application. 23.3% of the patients (n=7) showed healed perforation after the 2 month follow up period. Whereas, 30% of the patients (n=9) showed incomplete closure following the procedure. When statistically comparing the uptake of collagen patch between the outcome groups, chi square value was found to be 30.00 which was significant, with a df=2 [8].
Discussion
Collagen patch closure is a simple, short, cost effective procedure. Fibrinogen based collagen adheres strongly to tissue, forming a waterproof membrane. Collagen helps maintain the integrity and resilience of the tympanic membrane, which is important in maintaining the physiological functions of normal tympanic membrane. According to this study, collagen was found to have 66.7 % success, making it a viable option for repair of small perforations. Traumatic (38.1%) and post-myringoplasty (19%) cases have shown a higher success rate compared to infective group (42.9%) [9].
The failed cases were mostly of infective origin and 30% was due to extrusion of collagen patch. However these can be minimized with proper postoperative antibiotic cover and care. The hearing improvement was assessed by comparing the A-B gap during follow up PTA with pre-operative air bone gap, the use of collagen patch in the defect showed significant improvement in hearing following the procedure.
No complications had been encountered in the study and patient compliance was comparatively better when compared to myringoplasty as it was less traumatic and less time consuming. Collagen patch technique is cosmetically better as t is incisionless and hence less painful. Collagen grafts are fully transparent and hence the margins of the perforations can be easily seen by the surgeons. It also facilitates monitoring of the postoperative events. The results of collagen patch repair are better than those of conventional myringoplasty or paper patching in the literatures. Some studies of patch materials to treat the tympanic membrane perforation are listed below Table 5 [10].
| Author | Country | Model | TMP dura- tion | Cause of TMP | Patch material (patients number) | Control group | Assessment methods | Result |
|---|---|---|---|---|---|---|---|---|
| Lee. et al., | South Korea | Human | Chronic | COM | Paper patch after trimming with CO2 laser (90) | None | Endoscopy audiometry | Healing rate (%): 52.2 Improvement of ABG in all the cases where the TM healed to normal status |
| Hakuba et al., | Japan | Human | Chronic | COM | Silicone film with bFGF and atelocollagen (87) | None | Endoscopyaudiometry | Healing rate (%): 92 Hearing threshold improvement by 10 dB or more in 51 patients 13.4 dB HL of average hearing improvement |
| Lou and He | China | Human | Acute. s days | Trauma | Gelfoam patch (30), Perforation edge- approximation with gelfoam patch (30) | No treatment | Endoscopyhealing time infection rate | Healing rate (%): 97. 97 (study groups). 85 (control group) (p>0.05) Healing time (days): 16:5.6 18:4.7 (study groups) and 30: +10.1 (control group) (p<0.05) Infection rate (%): 3.3 (study groups). 7 (control group) |
| Saliba and Woods | Canada | Human | Chronic 6 months | COM | Hyaluronic acid fat graft myringoplasty (131) | Underlay technique with TF/TP, overlay technique with TF/ TP | Endoscopyaudiometry | Healing rate (%): 92.7 (study groups). 92.2 and 92.6 (control groups). (p>0.05) ABG (dB HL): Clinically and statistically significant improvement in hyaluronic acid fat graft myringoplasty |
| Araujo. et al. | Brazil | Human | Chronic | COM | Myringoplasty with polylysine latex biomembrane (39) | Myringoplasty only myringoplasty with silicone film | Endoscopy audiometry | Healing rate (%): 74.4 (study group). 70 and 57.1 (control groups) (p>0.05) Vascularization: Significantly greater in myringoplasty with polylysine latex biomembrane ABG (dB HL): 23.5-12.9" (study group). 25.2-11.9" and 28.5-10.1* (control groups) (p>0.05) |
| Jun, et al., | South Korea | Human | Acute, <3 months | Trauma | Egg shell membrane (39) | Perforation edge approximation | Endoscopy healing time | Healing rate (%): 92.3 (study group). 89.7 (control group) (p=0.74) Healing time (days): 42.8* 19.8 (study group). 87.2 4 41.3 (control group) (p=0.02) |
| Simsek and Akin, | Turkey | Human | Acute, <10 days | Trauma | Paper patch (33) | No treatment | Endoscopyaudiometry | Healing rate (%): 90.9 (study group). 76.7 (control group) (p>0.05) ABG (d8 HL): 23.6-1* (study group), 26.1-5* (control group) (p<0.001) |
| Present study | South Korea | Human | Acute and chronic>14 days | Trauma | Fibrinogen based collagen fleece (29) | None | Endoscopy audiometry | Healing rate (%): 100 ABG (dB HL): 12.9-2.4" |
Note: Preoperative average ABG→postoperative average ABG; TMP: Tympanic Membrane Perforation; COM: Chronic Otitis Media; ABG: Air Bone Gap; TM: Tympanic Membrane; TF: Temporalis Fasciz; TP: Tragal Perichondrium; BFGF: Basic Fibroblast Growth Factor
Table 5: Studies of patch material for tympanic membrane perforation treatment.
Conclusion
In this study, we found that using collagen patch as a graft material for the repair of small tympanic membrane perforations is effective. The postoperative air bone gap differed significantly from the preoperative. Furthermore, the technique requires no hospitalization, and can be used to avoid traditional tympanoplasty in cases with small perforations.
References
- Kristensen S (1997) Spontaneous healing of traumatic tympanic membrane perforations in man: a century of experience. J Laryngol Otol 106:1037-1050.
[Crossref] [Google Scholar] [PubMed]
- Chun SH, Lee DW, Shin JK (1999) A clinical study of traumatic tympanic membrane perforation. Korean J Otolaryngol Head Neck Surg 42:437-441.
[Crossref] [Google Scholar] [PubMed]
- Lee SH, Jin SM, Lee KC, Kim MG (2008) Paper patch myringoplasty with CO2 laser for chronic TM perforation. Eur Arch Otorhinol 265:1161-1164.
[Crossref] [Google Scholar] [PubMed]
- Hakuba N, Iwanaga M, Tanaka S, Hiratsuka Y, Kumabe Y, et al. (2010) Basic fibroblast growth factor combined with atelocollagen for closing chronic tympanic membrane perforations in 87 patients. Otol Neurotol 31:118-121.
[Crossref] [Google Scholar] [PubMed]
- Lou ZC, He JG (2011) A randomised controlled trial comparing spontaneous healing, gel foam patching and edge approximation plus gel foam patching in traumatic tympanic membrane perforation with inverted or everted edges. Clin Otolaryngol 36:221-226.
[Crossref] [Google Scholar] [PubMed]
- Saliba I, Woods O (2011) Hyaluronic acid fat graft myringoplasty: A minimally invasive technique. Laryngoscope 121:375-380.
[Crossref] [Google Scholar] [PubMed]
- Araujo MM, Massuda ET, Hyppolito MA (2012) Anatomical and functional evaluation of tympanoplasty using a transitory natural latex biomembrane implant from the rubber tree Hevea brasiliensis. Acta Cir Bras 27:566-571.
[Crossref] [Google Scholar] [PubMed]
- Jun HJ, Oh KH, Yoo J, Han WG, Chang J, et al. (2014) A new patch material for tympanic membrane perforation by trauma: The membrane of a hen egg shell. Acta Otolaryngol 134:250-254.
[Crossref] [Google Scholar] [PubMed]
- Levenson MJ (1998) The Management of traumatic perforation of tympanic membrane. Surg Otolaryn Med Pub 95-107.
- Gerhart J, Elder J, Neely C, Schure J, Kvist T, et al. (2006) MyoD-positive epiblast cells regulate skeletal muscle differentiation in the embryo. J Cell Biol 175: 283-292.
[Crossref] [Googlescholar] [IPubMed]