Case Report, Arch Transplant Vol: 1 Issue: 1
Lymphoid Interstitial Pneumonia in a Renal Transplant Recipient
Emma Bray1, Claire Molloy1, Vijaya Bharath Ramasamy1, Olexandra Kozyar1 and Shafi Malik2*
1Department of Renal and Transplantation Medicine, University Hospital Wales, Heath Park, Cardiff, United Kingdom
2Consultant Nephrologist and Transplant Physician, John Walls Renal Unit, Leicester General Hospital, United Kingdom
*Corresponding Author : Shafi Malik
Consultant Nephrologist and Transplant Physician, John Walls Renal Unit, Leicester General Hospital
University Hospitals of Leicester NHS Trust, United Kingdom
Tel: +441162584131
E-mail: dr_shafi@hotmail.com
Received: May 11, 2017 Accepted: May 31, 2017 Published: June 06, 2017
Citation: Bray E, Molloy C, Ramasamy VB, Kozyar O, Malik S (2017) Lymphoid Interstitial Pneumonia in a Renal Transplant Recipient. Arch Transplant 1:1.
Abstract
Objectives: A case report of lymphoid interstitial pneumonia (LIP) in a renal transplant patient who is immunosuppressed with tacrolimus.
Background: LIP is a rare lymphoproliferative disorder affecting the lungs. It is described in the literature as: diffuse infiltration of the alveolar septa by dense collections of lymphocytes and a mixture of plasma cells and other elements. LIP is associated with several conditions, most of which affect the immune system. The development of this condition following immunosuppression with sirolimus is mentioned in the literature but there are currently no documented cases on the development of LIP following treatment with tacrolimus.
Methods: Case report and literature review.
Results: A 44 year old lady with rapidly progressing renal failure secondary to IgA nephropathy developed progressive dyspnoea nine years after a cadaveric renal transplantation. She was immunosuppressed on tacrolimus. Plain chest film revealed bilateral interstitial infiltrates. Following open lung biopsy she was diagnosed with lymphoid interstitial pneumonia and made a good recovery after treatment with Prednisolone.
Conclusion: LIP is a rare complication of treatment with tacrolimus, to our knowledge this is the first reported case of this condition in a patient maintained on tacrolimus. A lung biopsy may be required as the differential diagnosis is vast and treatment with prednisolone can lead to good outcome.
Keywords: Lymphoid; Pneumonia; Renal Transplant; Immunosuppression
Introduction
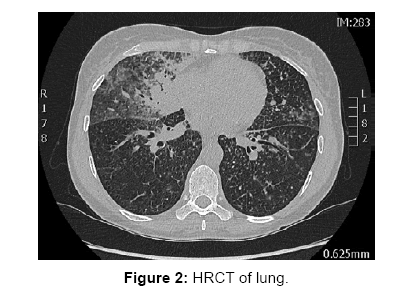
Here we report a case of a patient with IgA nephropathy who developed lymphoid interstitial pneumonia (LIP) 11 years after her renal transplant. Initially identified by Liebow and Carrington, LIP, a rare disorder, was described as a ‘benign lymphoproliferative disorder found in the lungs’ [1]. They described it as: “diffuse infiltration of the alveolar septa by dense collections of lymphocytes and a mixture of plasma cells and other elements”. This description further evolved into “a hypoplastic disorder of the mucosa associated lymphoid tissue, affecting the lungs”. LIP is associated with several conditions, notably common variable immune deficiency (CVID), Sjogren’s syndrome, post bone marrow transplantation as graft versus host disease, AID’s, Epstein-Barr virus infection and related to hypogammaglobulinaemia [2-5] In renal transplant recipients, LIP has been associated with sirolimus immunosuppression but there have been no reports of association with calcineurin inhibitors (CNI) [6,7]. The patient presented to our transplant centre where we proceeded to do a high-resolution computed tomography (HRCT) scan (Figure 1). This showed bilateral hilar lymphadenopathy (BHL), mediastinal lymphadenopathy, multiple nodules in left lung and right base, interlobular septal thickening in both the middle and lower right lobe and ground glass change in right middle lobe.
Case Report
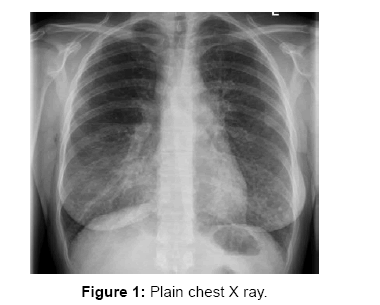
This 44 year old retired air stewardess developed rapidly progressive renal failure secondary to IgA nephropathy in 2005, and underwent a successful deceased donor renal transplant in 2006. She has no other past medical history, and was immunosuppressed on single agent of tacrolimus. She remained fit and well until late 2014, when she presented to her primary care physician with a six week history of a dry cough and progressive shortness of breath. She was uncomplaining of other symptoms. Her symptoms were initially treated as a lower respiratory tract infection with co-trimaxazole and later doxycycline, but this failed to improve her condition. Her inflammatory markers remained within the normal parameters (CRP<5 mg/dl) but a plain radiograph of her chest (Figure 2) revealed bilateral interstitial infiltrates.
An urgent broncho alveolar lavage, (BAL) was performed, to exclude pneumocystitis jiroveci pneumonia (PJP) among other opportunistic pathogens. Interestingly the PJP polymerase chain reaction, (PCR), was negative from her BAL but her serum EBV PCR was positive at moderate titres, she was previously negative for serum EBV PCR at pre-transplant stage. After consulting our local microbiology and respiratory physicians for advice, the EBV viremia was thought to be an incidental finding and unlikely to explain her radiological appearances and the clinical features.
The patient’s lack of clinical improvement with antibiotics and lack of clear etiology for the extensive changes in the HRCT combined with concerns about possible post-transplantation lymphoproliferative disorder (PTLD) led us to perform an open lung biopsy. Histology of this biopsy was described as “widespread granulomatous nonnecrotising lesions”. Our differential included sarcoidosis and LIP. Prednisolone was initiated and pateint made good recovery and was discharged home with a plan to taper prednisolone. On review of the HRCT the appearances are typical of LIP.
Discussion
LIP is a rare lung disorder that is usually associated with connective tissue disorders and infections. It is rarer in transplant patients but has been reported in patients maintained on sirolimus immunosuppression. To our knowledge this is the first case of LIP related to tacrolimus, in difficult to diagnose cases an open lung biopsy may be needed to diagnose the condition.
References
- Liebow AAC, Carrington CB (1969) The Interstitial Pneumonias In: Frontiers of Pulmonary Radiology, Grune & Stratton, New York.
- Silva CI, Flint JD, Levy RD, Muller NL (2006) Diffuse lung cysts in lymphoid interstitial pneumonia: high-resolution CT and pathologic findings. J Thorac Imaging 21: 241-4.
- Lymphocytic interstitial pneumonia in primary Sjogren syndrome. Pneumonol Alergol Pol 73: 277-80.
- Non-specific interstitial pneumonia as a manifestation of graft-versus-host disease following pediatric allogeneic hematopoietic stem cell transplantation. Pathol Int 60: 137-42.
- Lymphocytic Interstitial Epub. Cystic lung disease interstitial lung disease interstitial lung disease in HIV-positive patients Interstitial lung disease in Sjogren syndrome Polyclonal lymphoid lung infiltrates Pseudolymphoma Pulmonary lymphoproliferative disorders. Pneumonia Clin Chest Med 37: 463-74
- Morelon E, Stern M, Israël-Biet D, Correas JM, Danel C, et al. (2001) Characteristics of sirolimus-associated interstitial pneumonitis in renal transplant patients. Transplantation 72: 787-90
- Ussavarungsi K, Elsanjak A, Laski M, Raj R, Nugent K (2012) Sirolimus induced granulomatous interstitial pneumonitis. Collection granulomatous interstitial pneumonitis interstitial pneumonitis pulmonary toxicity renal transplantation Sirolimus. Respir Med Case Rep 7: 8-11.