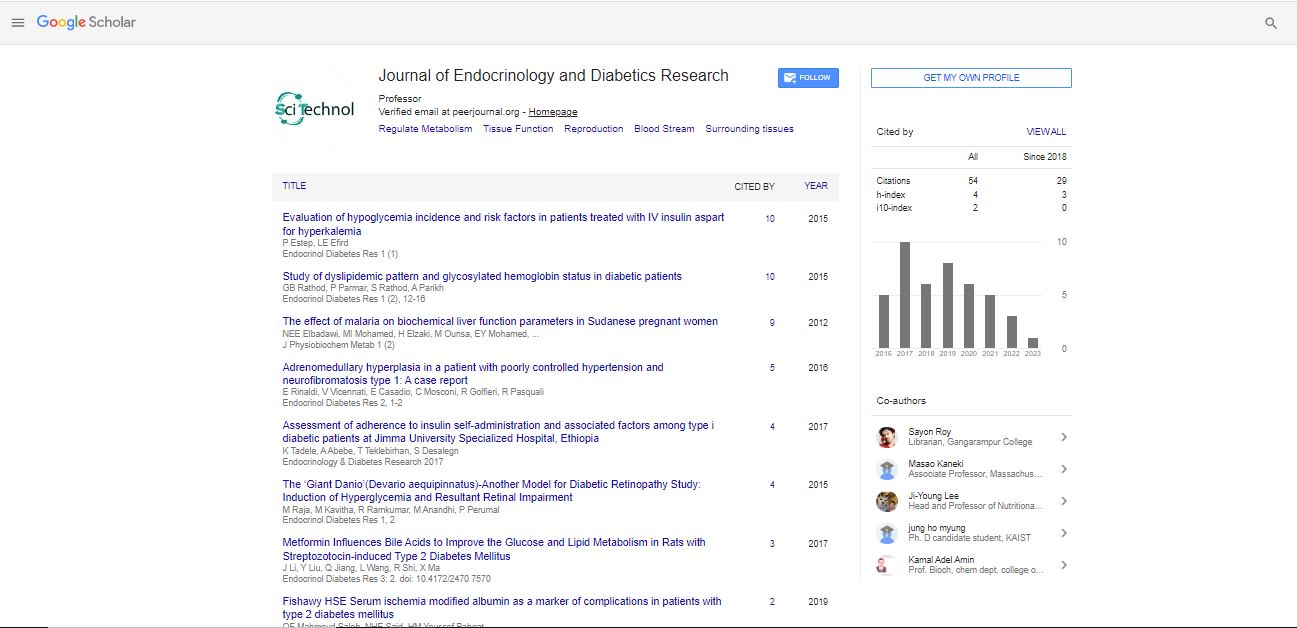
Commentary, Endocrinol Diabetes Res Vol: 8 Issue: 1
Maturity Onset Diabetes of Young Type 5: Diabetes with Extra Pancreatic Features
Adnan Haider1*, Oksana Symczyk1, Ayesha Hasan1, Dylan Holland1, Muhammad Atif khan2
1Department of Medicine, West Virginia University, Morgantown, USA
2Department of Endocrinology, Ohio State University, Morgantown, USA
*Corresponding Author:Adnan Haider
Department of Medicine, West Virginia University, Morgantown, USA, E-mail: adnan.haider@hsc.wvu.edu
E-mail: adnan.haider@hsc.wvu.edu
Received Date: 31 December, 2021, Manuscript No. ECDR-21-38457;
Editor assigned Date: 03 January, 2022; Pre QC No. ECDR-21-38457 (PQ);
Reviewed Date: 14 January, 2022, QC No. ECDR-21-38457;
Revised Date: 18 January, 2022, Manuscript No: ECDR-21-38457 (R);
Published Date: 31 January, 2022, DOI:10.4172/2324-9323.1000315
Abstract
This case involves presenting new-onset diabetes diagnosed during pregnancy in a patient with congenital dysplastic right kidney. Case report: Clinical presentation, biochemical features, imaging in a patient with diabetes diagnosed during pregnancy and congenital dysplastic right kidney. Discussion: We present a case of a 22-year-old female with congenital dysplastic right kidney diagnosed with Gestational Diabetes mellitus after failing a 1- hour oral glucose tolerance test, requiring insulin during pregnancy. Because of family history of diabetes and morphologic renal abnormalities at young ages on the maternal side of the family, our patient was evaluated for maturity-onset diabetes of adult and was found to have HNF-1β mutation. Conclusion: This case highlights the importance of considering the diagnosis of maturity-onset diabetes of young and particularly MODY-5 in individuals with extrapancreatic features. MODY-5 should also be considered in a patient undergoing renal transplant at young ages with a family history of morphologic renal abnormalities.
Keywords: Gestational diabetes, Dysplastic kidney, HNF-1B
Introduction
MODY-5 is caused by an autosomal dominant mutation in the HNF1b gene. Our objective is to report a case of a young female with a history of dysplastic right kidney, diagnosed with gestational diabetes. Morphologic kidney abnormalities, electrolyte abnormalities (low magnesium and high urate), strong family history of diabetes and renal abnormalities at young ages should alert the clinician of this diagnosis.
Case Report
A previously healthy 22-year-old female was diagnosed with Gestational Diabetes after failing her 1-hour glucose tolerance test at
28 weeks gestation with a blood glucose level of 241. Elevated glucose levels were noted on random basic metabolic panels done
prior to pregnancy, but not meeting criteria to diagnose diabetes mellitus. Patient had no other symptoms at the time of the abnormal oral glucose tolerance test. Pertinent past medical history prior to pregnancy included ultrasounds showing a small multicystic dysplastic right kidney. Patient’s left kidney showed compensatory Hypertrophy and a small midpole cyst. Kidney function is followed by nephrology and has been unremarkable. Family history is positive for polycystic kidney disease in her mother and maternal grandmother.
Due to her diagnosis of gestational diabetes, prior elevated glucose readings, and pertinent past medical history, a polycystic disease panel was performed to test for Mature Onset Diabetes of the Young (MODY). This panel came back positive for a pathologic mutation to HNF-1β with a deletion of exon 1-9 with genomic coordinates chr17:36047329_36105161 (GRCh37). The patient was subsequently diagnosed with MODY5. Patient was originally managing glycemic control with diet and exercise but eventually was placed on Basal Insulin and titrated to meet the glycemic targets during pregnancy. Patient has required no insulin since giving birth to her baby [2]. Patient did experience other extra-pancreatic symptoms that included low magnesium (1.3mg/dl), high uric acid (11.1mg/dl), and pancreatic hypoplasia noted on previous CT done two years prior to her diagnosis. CT scan was done to rule out renal stones and did show pancreatic tail hypoplasia. Patient most recent blood work done 6 weeks following delivery. She delivered a healthy baby girl via spontaneous vaginal delivery at 39 weeks of gestation weighing 3170 g with APGAR score of 8 and 9 at 1 and 5 minutes respectively. Her daughter is born with normal kidney.
Discussion
Monogenic forms of diabetes result from a single gene defect with an autosomal dominant pattern of inheritance. A high index of suspicion based on strong family history of diabetes at young ages in at least three generations is suggestive of this diagnosis which can affect successful patient management, ensure healthy pregnancy in female patients and offering genetic counselling to the families. To date, fourteen different genes have been implicated in the etiology of MODY. GCK mutation is the most common culprit mutation accounting for 30-50% of all MODY. Hepatic nuclear factor 1B gene identified in patients with MODY-5 comprises less than 5% of MODY subtypes. Although the exact prevalence is not known, current estimates suggest that 1–5% of all diabetes cases in the United States and other developed countries are a monogenic form of diabetes. Often the diagnosis is overlooked and misdiagnosed as diabetes type 1 or type 2 and therefore the true prevalence of MODY may be higher. Given the absence of a typical phenotype and the cost of genetic analysis, it is indeed a challenge to distinguish MODY from many people with young-onset type 2 and type 1 diabetes. Patients with MODY are often misdiagnosed as type 2 diabetes, mainly if hyperglycemia was first detected in adulthood. Several reasons like the increasing prevalence of diabetes among youths, positive family history of diabetes, lack of characteristic clinical features and therapeutic response to insulin secretagogues add to this confusion. Similarly, if they present in their early teens, the default diagnosis is usually type 1 diabetes, and they are put on insulin, sometimes with multiple daily injections a day. Most MODY types do not involve extra pancreatic organs; in contrast, MODY-5 frequently comprises extra pancreatic organs. The first case of MODY-5 was reported in 1997 in a Japanese family. The HNF-1β is encoded by the human transcription factor 2 gene and is expressed in a wide variety of tissues, including the kidney, pancreas, genitourinary epithelium, liver, and lung during embryogenesis. HNF1B-associated MODY is a multisystem disease and includes genital tract malformation, abnormal liver function test, hypomagnesemia and hyperuricemia associated early gout; neurological features like autism spectrum disorders and cognitive impairment are also seen in MODY-5. Renal cysts are the most frequently detected feature of HNF-1β associated kidney disease, and MODY 5 is also known as renal cysts and diabetes (RCAD) syndrome. Patients with a strong family history of diabetes at young ages and renal morphologic abnormalities diagnosed at or soon after birth should be considered for the HNF1B screen. Diabetes prevalence was 80%, and that of renal malformations was 91% in HNF-1β mutation. Diabetes can present with weight loss, polyuria, and polydipsia in about half of the patients; ketoacidosis was the initial presentation in 5% of the patients. A1c profile in MODY-5 patients showed A1c ranging from < 7 % in one-third of the patients to > 13 % in another 35% of the patients at the initial diagnosis. Pancreatic hypoplasia with resulting beta-cell hypoplasia results in decreased Insulin secretion and release, altered glucose- sensing and increased hepatic insulin resistance also play a major role in the development of diabetes. Severity of pancreatic hypoplasia determines the severity of hyperglycemia and possibility of ketoacidosis at initial presentation. Imaging of the pancreas is therefore helpful in MODY-5 patients. Nongenetic factors that affect Insulin sensitivity (infection, puberty, pregnancy and rarely Obesity) can trigger diabetes onset and affect the severity of hyperglycemia in MODY but do not play a significant role in the development of MODY. Renal functional decline is reported; a median yearly decrease in the estimated glomerular filtration rate (eGFR) of 2.45 ml/min/1.73 m2 was observed in a study of 27 adults with an HNF-1β mutation and a wide variety of renal phenotypes. MODY- 5 patient who develops ESRD should be considered for renal transplantation; however, these patients are at increased risk of developing Post-transplant diabetes mellitus. Like Type 1 Diabetes patients requiring renal replacement therapy, HNF-1β patient should be considered for simultaneous pancreatic and renal transplant. Functional renal anomalies notably hypomagnesemia and hyperuricemia are also seen in MODY -5 patients. HNF-1β transcription function over the FXYD Domain Containing Ion Transport Regulator 2 (fxyd2), gene that encodes sodium-potassium ATPase in the distal convoluted tubule, which plays an important role in magnesium reabsorption. HNF-1β is also responsible for transcription of uromodulin gene which is involved in urate transport. Unlike asymptomatic hypomagnesemia, elevated uric acid levels can present as symptomatic monoarticular gout. Primary hyperparathyroidism has been identified because HNF-1β inhibits the transcription of parathormone hormone.