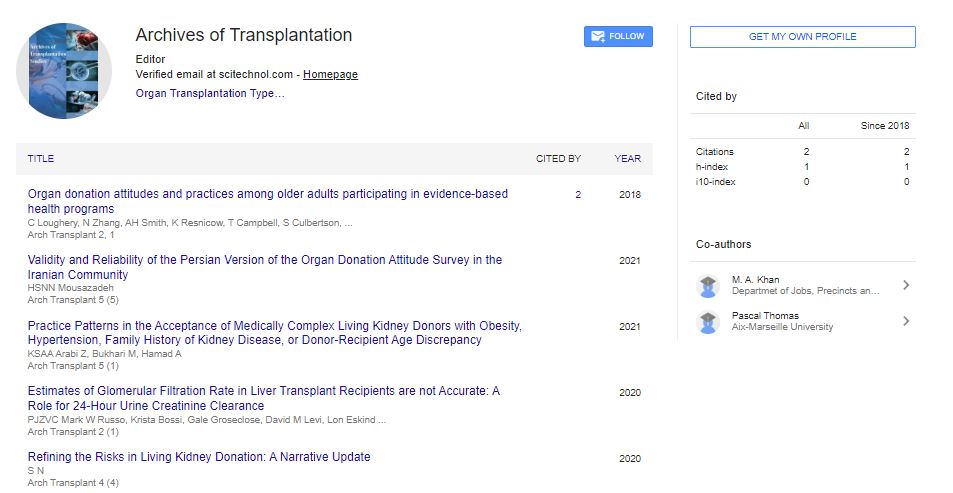
Research Article, Arch Transplant Vol: 4 Issue: 5
Organ Donation Attitudes and Practices Among Older Adults Participating in Evidence-Based Health Programs
Caitlin Loughery1*, Nanhua Zhang2, Allyce Haney Smith3, Ken Resnicow4, Taneisha Campbell5, Suzanne Culbertson1, Pratima Sharma6 and Ann M Andrews1
1National Kidney Foundation of Michigan, Ann Arbor, MI 48109, United States
2Cincinnati Children’s Hospital and University of Cincinnati, Cincinnati, OH 45221, United States
3Greenfield Health System, Bingham Farms, MI 48025, United States
4Department of Health Behavior and Health Education, University of Michigan School of Public Health, Ann Arbor, MI 48109, United States
5Gift of Life Michigan, Ann Arbor, MI 48108, United States
6Division of Gastroenterology and Hepatology, Michigan Medicine, University of Michigan, Ann Arbor, MI 48109, United States
*Corresponding Author : Caitlin Loughery
National Kidney Foundation of Michigan, 1169 Oak Valley Drive, Ann Arbor, MI, 48108, USA
Tel: 734-222-9800
E-mail: cbuechley@nkfm.org
Received: February 26, 2018 Accepted: June 22, 2018 Published: June 30, 2018
Citation: Loughery C, Zhang N, Smith AH, Resnicow K, Campbell T, et al. (2018) Organ Donation Attitudes and Practices among Older Adults Participating in Evidence-Based Health Programs. Arch Transplant 2:1.
Abstract
Objective: The study assessed attitudes, barriers, and practices related to deceased organ donation and intent to enroll on a donor registry among older adults in health programs. Methods: We surveyed 1,286 adults (71% over age 60) participating in evidence-based self-management/lifestyle change programs in Michigan about their attitudes toward organ donation. Results: Three subscales with good psychometric properties were identified: General Benefits (Alpha .83), General Barriers (Alpha .79), and Age/Health Barriers (Alpha .61). Female gender, white race, higher education attainment/income, and intent to sign up on the donor registry were correlated with positive attitudes toward donation. Participants cited age and chronic disease status as barriers to enrolling as organ donors. Conclusion: Education on donor eligibility and perceived barriers could increase organ donation rates among participants in evidence-based health programs.
Keywords: Transplant; Organ donation; Age; Attitudes; Chronic illness; Selfmanagement; Validated survey
Abbreviations
OPTN: Organ Procurement and Transplantation Network; OPO: Organ Procurement Organization; CDSMP: Chronic Disease Self- Management Program; DSMP: Diabetes Self-Management Program; DPP: National Diabetes Prevention
Introduction
Organ transplantation is an effective and viable treatment option for those with end stage organ failure; it can be their only chance for longer life. However, registration rates on the organ donor registry do not meet the growing demand for organs [1]. According to Organ Procurement and Transplantation Network (OPTN) data, 5,800 people died on the waiting list in 2017. Many others have long wait times; 72% of those waiting for a kidney wait for over a year, and 15% wait longer than five years. Over 80% of those on the waitlist are waiting for a kidney [2]. As of May 2018, there have been nearly 186,000 deceased kidney donors nationally, according to OPTN data. The majority of these donations occur in California, Texas and Pennsylvania (10.8%, 7.9% and 7.5%, respectively). Among these deceased kidney donors, nearly 80% are between the ages of 18-64. Donors that are 65 and older comprise only 5.9% of this number.
Data suggest that those over the age of 65 are less likely to sign up on the registry compared to those aged 18-34 years [3]. Misconceptions about eligibility due to age and chronic illness status are common barriers to signing up on the registry [4]. Data from the 2012 National Organ Donation Survey showed that 16.5% of those not registered to donate but not opposed to future registration indicated that they were too old or not healthy enough to donate [3]. Lack of willingness to donate among older adults could be attributed to the belief that age and health status prevented them from donating [5]. Older adults lacked adequate information about age and health status as it relates to organ donation; however, many older adults had positive feelings about organ donation and were even more comfortable thinking about death and the benefits that organ donation would have on their family compared to their younger cohorts. Quick and colleagues detail the “attitude-registration discrepancy” among mature adults (aged 50-64 years) and explore three models to try to account for the discrepancy [6].
One approach to increasing organ donation has been through the use of social media and online messaging. This approach has had some success in increasing organ donor registration [7]. However, this medium does not adequately reach older populations. Although social media usage is increasing among older adults, most are still not using it. Only 35% of adults age 65 and older report using social media, as compared to 90% of young adults age 18-29 [8].
Furthermore, there are marked differences in consent rates for organ donation among potential brain-dead donors across age groups [9]. In an analysis of Organ Procurement Organization (OPO)- reported eligible deaths from 2008-2011, lower rates of consent were observed among families of older potential donors, particularly those ≥ 55 years [9]. This finding aligns with other studies demonstrating lower consent rates among older potential donors in a single U.S. OPO and the Netherlands [10,11]. These findings highlight a need to identify a mechanism for increasing consent rates among this age group.
In Michigan, more than 62% of adult residents are signed up on the donor registry; this means that more than one-third of the adult population is not signed up [12]. An increase in registration rates would increase the number of organs available for transplant and shorten waiting times. The current study investigates organ donation attitudes and beliefs among adults participating in evidence-based health programs. The measure used was developed by our group to specifically address the barriers of age and health condition, which builds upon our previous research on organ donation.
Methods
A research consortium consisting of the National Kidney Foundation of Michigan (NKFM), the University of Michigan School of Public Health, and Gift of Life Michigan/Minority Organ and Tissue Transplant Education Program designed and implemented the study. It was part of a larger trial called Leave a Legacy of Life, which evaluated the effectiveness of providing peer education about organ donation to evidence-based health program participants, many of whom are over 50 with a chronic condition. The trial utilized a cluster randomized, pre-post study design with a comparison group. Data was obtained from the baseline survey, which was completed by 1,286 participants at 139 health workshops between July 2015 and February 2017 in southcentral, southeast, and west Michigan. Further detail on survey content can be found in (Table 1). The study was approved by the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board.
| Item | Rotated Factor Loading | |
|---|---|---|
| Scale 1: General Benefits (Alpha .83) | 1. Signing up to donate my organs will allow my family to carry out my wishes | 0.60 |
| 2. Donating my organs is consistent with my religious tradition. | 0.47 | |
| 3. Signing up to donate my organs is a way I can do something good for others. | 0.67 | |
| 4. Donating my organs can help my family cope with their grief. | 0.62 | |
| 5. Signing up to donate my organs can help my family by removing the stress of making that decision. | 0.71 | |
| 6. Donating my organs allows me to help others live | 0.76 | |
| 7. Organ donation allows something positive to come out of a person’s life. | 0.79 | |
| 8. Donating my organs may provide my family with some comfort. | 0.73 | |
| Scale 2: General Barriers (Alpha .79) | 9. It costs a donor’s family money to donate organs. | 0.50 |
| 10. Even thinking about death could bring about bad things. | 0.63 | |
| 11. Organ donation is against the rules of my religion. | 0.61 | |
| 12. If a person has donated his or her organs, it is impossible for that person to have a regular funeral service. | 0.52 | |
| 13. If I signed up to donate my organs, my family members would not approve. | 0.54 | |
| 14. A person needs to have all their parts in order to go to heaven. | 0.62 | |
| 15. It would be weird to have my organs inside of someone else. | 0.61 | |
| 16. I can’t decide whether I want to donate my organs until I know more about brain death. | 0.51 | |
| 17. If a person has signed the organ donor registry, doctors won’t try as hard to save that person’s life. | 0.58 | |
| 18. Doctors give preference to white people over people of color or minorities when deciding who will receive an organ. | 0.53 | |
| Scale 3: Age/Health Barriers (Alpha .61) | 19. People over the age of 50 cannot be organ and tissue donors. | 0.43 |
| 20. If a person has a health condition (asthma, diabetes, etc), then they cannot be an organ donor. | 0.61 | |
| 21. There are age restrictions on being an organ donor. | 0.66 | |
| 22. Anyone can be a donor regardless of their age or medical condition. | 0.73 |
Table 1: Survey questions, subscale grouping, and factor loading.
Survey development
The survey instrument was adapted from the instrument used by the research consortium in previous studies conducted among churches [13], alumni chapters of historically African American Greek organizations [14], and dialysis centers. The original 18-item scale was tested among 1,225 members of 21 African American churches in Southeast Michigan; three subscales with good psychometric properties were identified: (1) Barriers; (2) Family/ Race Benefits; and (3) Altruism [13]. The original scale was adapted slightly for each study population. For the current study, we adapted the instrument for use among older adults with a chronic condition. Changes were made based on input from workshop leaders, patients, and consortium members with expertise in instrument design. Four new items (Table 1) were added to the survey which probes how age and chronic health condition affect one’s ability to donate. In addition, two new items asked about whether discussing organ donation at a health management workshop is “appropriate” or “good”.
Survey items assessed participants’ benefits and barriers to organ donation. Benefits include altruism, providing comfort to family members after death, and religious beliefs. Barriers include family disapproval, cost, religious and spiritual beliefs, misconceptions about the donation process, and the “ick” and “jinx” factors. Ick factors describe feelings of disgust toward the organ donation and transplantation process, while jinx factors describe the fear or superstition that signing up to be a donor could lead to harm or premature death [15]. Response options were scaled 1 ‘strongly disagree’ to 7 ‘strongly agree’.
Baseline measurements
Baseline measurements included attitudes toward organ donation, enrollment status on the Michigan Organ Donor Registry, intention to sign up to be a donor, and demographics. These measurements were collected from the baseline survey and are self-reported.
Enrollment status on the Michigan Organ Donor Registry was assessed through the questions, “Which, if any, of the following methods have you used to sign up to be an organ donor?” and “Do you have a red heart sticker on your Michigan Driver’s License or State ID card?” A positive response to the red heart sticker question indicated positive donation status. In the state of Michigan, the red heart signifies enrollment on the Donor Registry.
Intention to donate was assessed through the question, “How likely are you to sign up as an organ donor?” Response options were scaled 1 ‘not at all likely’ to 10 ‘very likely’. Participants who answered ‘Yes’ to having a red heart sticker on their license were instructed to skip this question.
Demographic data included date of birth, gender, race/ethnicity, education, and income. Educational status was determined by asking, “What is the highest grade or degree you have completed?” Response categories were ‘Some high school or less’, ‘High school graduate or GED’, ‘Some College or 2 year degree’, ‘4-year college graduate”, ‘Master’s Degree’, and ‘Doctoral or professional degree’.
Household income was assessed through the question, “What is your current monthly household income after taxes? (Please include income from all sources in your home)”. This question was marked as optional. Response categories were ‘under $1,000’, ‘$1,000-$1,999’, ‘$2,000-$2,999’, ‘$3,000-$4,999’, ‘$5,000-$6,999’, ‘$7,000-$8,999’, ‘$9,000-$10,999’, ‘$11,000-$16,999’ and ‘$17,000+’. Responses were collapsed into smaller categories as displayed in (Table 2).
| Intervention (n=750) |
Control (n=536) |
Total (n=1286) |
|
|---|---|---|---|
| Age Group (%) | |||
| 45 or less | 4.93 | 6.20 | 5.45 |
| 45-60 | 24.06 | 22.93 | 23.59 |
| >60 | 71.01 | 70.87 | 70.95 |
| Gender (Female %) | 80.33 | 82.80 | 81.21 |
| Race (%)a | |||
| Black | 28.88 | 35.86 | 31.78 |
| Hispanic/Latino | 1.48 | 1.71 | 1.58 |
| White | 66.13 | 55.60 | 61.75 |
| Other | 3.51 | 6.83 | 4.89 |
| Education (%) | |||
| Some high school or less | 4.20 | 4.74 | 4.43 |
| High school or GED | 24.80 | 21.63 | 23.48 |
| Some college or 2-year degree | 38.08 | 37.95 | 38.02 |
| 4-year college | 18.16 | 19.92 | 18.89 |
| Master’s degree or above | 14.77 | 15.75 | 15.18 |
| Monthly Income (%) <$2,000 $2,000-4,999 $5,000 or more |
29.86 34.89 35.25 |
25.58 29.20 45.22 |
28.10 32.56 39.34 |
| Diabetes (yes %) | 46.82 | 40.28 | 43.88 |
| High BP (yes %) | 61.63 | 60.58 | 61.19 |
| Health insurance (yes %) | 99.33 | 99.35 | 99.34 |
| Mean Scale 1: General Benefits (Mean, SD) | 5.23 (1.33) | 5.20 (1.38) | 5.22 (1.35) |
| Mean Scale 2b: General Barriers (Mean, SD) | 5.86 (1.04) | 5.83 (1.10) | 5.85 (1.07) |
| Mean Scale 3b: Age/Health Barriers(Mean, SD) | 5.05 (1.38) | 5.04 (1.38) | 5.05 (1.38) |
| Rate of Positive Donation Statusa | 39.06 | 33.02 | 36.56 |
| Positive Intended Donation Status Low (1-3) Medium (4-7) High (8-10) |
39.33 41.25 19.42 |
39.26 39.57 21.17 |
39.30 40.51 20.19 |
| Number of Patients per Workshop (mean, range) | 8.79 (2-17) | 9.49 (1-22) | 9.19 (1-22) |
bSome items reversely coded so that higher score means pro-donation.
Table 2: Participant Demographics and Baseline Information.
Setting
Surveys were administered at three evidence-based health programs implemented by the NKFM: the Chronic Disease Self- Management Program (CDSMP), the Diabetes Self-Management Program (DSMP), and the National Diabetes Prevention Program (DPP). The CDSMP and DSMP are six-week workshops developed by Stanford University that provide skills and tools to help people living with chronic conditions take an active role in managing their health. Participants in CDSMP/DSMP workshops have at least one chronic condition and/or are a caregiver for a loved one with a chronic condition [16,17]. Information about the program’s availability can be found on the Evidence-Based Leadership Council website (www. eblcprograms.org). The DPP is a year-long program developed by the Centers for Disease Control and Prevention. It promotes lifestyle changes, including healthy eating and increased physical activity, among people with a diagnosis of prediabetes and/or who are at risk for developing type 2 diabetes [18]. Information about the program’s availability can be found www.cdc.gov/diabetes/prevention. These programs reach older adults with chronic conditions and provide a “safe space” for open discussion about health and personal matters, including sensitive topics such as deceased organ discussion. Adding onto evidence-based programs allowed a preexisting structure to facilitate discussion in a way that allowed the information to be easily accepted by the participants.
Program workshops are generally held in community locations, including hospitals, senior centers, churches, libraries, and assisted living communities. Workshops were randomized into an intervention (organ donation education) or control (education on another health topic) group. Prior to randomization, workshops were pair matched based on program type (CDSMP/DSMP or DPP), income level (<$35,000 or >$35,000), and race demographics (majority white, >35% African American, or >15% Hispanic/Latino). Income level and race demographics were based on zip code data from the workshop location. Baseline survey administration was uniform for both intervention and control workshops. Participants were asked if they had diabetes and/or hypertension. Insurance status was also collected on the baseline survey.
Survey administration
A program coordinator administered consent forms and baseline surveys during week one and/or two of the CDSMP/DPSMP and during week five and/or six of the DPP. The paper survey usually took participants 15 to 20 minutes to complete. The coordinator was present and available to answer questions throughout the course of the survey. Eligible participants were any person enrolled in the workshop who was legally competent to give informed consent. Workshops ranged in size from one to 22 persons, and each participant who opted to fill out a baseline survey was given a $10 gift card to a local grocery store.
Surveys were coded with unique identification numbers grouped by survey location and workshop type. Identifying participant information associated with these unique numbers was stored in both separate databases and separate physical locations to enable followup survey results and tracking of registration in the Michigan Organ Donor Registry, while still protecting confidentiality.
Statistical analysis
Factor analysis, with varimax rotation, was used to identify potential subscales. After identifying a three factor solution, we computed internal consistency of each scale (Cronbach’s Alpha) and then examined the relationship between scale scores, demographics, and intended donor status. Three subscales were identified, and the associations between scale scores, demographics, and intended donor status were examined. Multivariate analyses were used to examine the association between each scale score and age, gender, race, education, income, chronic conditions, insurance status, current donation status, and intended donation status. All models accounted for the effect of sampling individuals from clusters (health program workshops) rather than randomly sampling individuals from the population. All p values adjust for the intraclass correlation (ICC) due to the design effect of sampling individuals within chapters. The ICCs of the two scales identified ranged from 0 to 0.002. The data analysis for this paper was conducted in SAS software, Version 9.3 (SAS Institute Inc., Cary, NC, USA).
Results
A total of 1,286 participants from 139 health workshops completed baseline surveys. Workshops averaged 9.3 participants. Among all participants approached (n=1,461) 88% agreed to participate in the survey. As seen in (Table 2), 71% of participants were over age 60 years. The majority of participants were female (81%), white (62%), and had some college education or greater (72%). Monthly household income was reported at under $5,000 for 61% of participants, and under $2,000 for 28% (Table 2).
Three unique subscales were identified in the rotated factor analysis: Scale 1-General Benefits (alpha .83), Scale 2-General Barriers (alpha .79), and Scale 3-Age/Health Barriers (alpha .61) (Table 1). Scale 1 contained 8 items, Scale 2 contained 10 items, and Scale 3 contained 4 items.
Several demographic variables and intended donation status were correlated with organ donation attitudes. On Scales 1 and 2, there were significant differences across gender and income. Female participants reported more positive attitudes toward organ donation on these two scales. Similarly, participants with a monthly income greater than $5,000 and between $2,000-$4,999 had more positive attitudes than those with monthly income less than $2,000 for these two scales. Across all three scales, there were significant differences across race and education. Participants with higher education level reported more positive attitudes, while white participants had more positive attitudes than other racial/ethnic groups. Participants with positive self-reported donation status had significantly more positive attitudes on all three scales. Greater intention to donate was associated with significantly more positive attitudes across all scales (Table 3).
| Mean Attitude (1: General Benefits) |
Mean Attitude (2: General Barriers)* |
Mean Attitude (3: Age/Health Barriers)* |
|
|---|---|---|---|
| Age 45 or less 45-60 >60 |
5.30 5.34 5.22 |
5.78 5.88 5.86 |
5.41 5.13 5.00 |
| Gender Male Female |
4.971 5.271 |
5.721 5.881 |
5.08 5.04 |
| Race Black Hispanic/Latino White Other |
4.841 4.98 5.471,2 4.612 |
5.471 5.612 6.071,2,3 5.573 |
4.791 4.552 5.191,2 5.02 |
| Education Some high school or less High school or GED Some college or 2-year degree 4-year college Master’s degree or above |
4.661,2,3 4.804,5,6 5.261,4 5.492,5 5.503,6 |
5.411,2 5.711,3 5.832 5.971 6.112,3 |
4.91 4.931,2 5.04 5.191 5.192 |
| Income <$2,000 $2,000-4,999 $5,000 or more |
4.861,2 5.331 5.442 |
5.701,2 5.921 5.972 |
5.03 5.15 5.13 |
| Diabetes Yes No |
5.09 5.29 |
5.78 5.88 |
4.99 5.07 |
| High BP Yes No |
5.26 5.18 |
5.88 5.87 |
5.07 5.09 |
| Insurance Yes No |
5.25 4.60 |
5.88 5.24 |
5.07 4.63 |
| Self-reported Donation Status Yes No |
5.711 4.951 |
6.241 5.681 |
5.431 4.841 |
| Intended Donation Status Low (1-3) Medium (4-7) High (8-10) |
4.401 5.111 5.561 |
5.491 5.532 6.111,2 |
4.641 4.712 5.511,2 |
Identical superscript means significant group difference in the least-squared means based on t-tests.
Table 3: Predictors/Correlates of Attitudes toward Donation – Participant (n=1286).
Participant responses to individual items on Scale 3 were analyzed for presence of misconceptions regarding age and health status. Half of participants (50.7%) disagreed with the statement, “Anyone can be an organ donor regardless of their age or medical condition” (Item 22). Regarding health condition, 39.2% responded between neutral to ‘Strongly Agree’ on Item 20. Similar results were found for Item 21 (36.1%) and Item 19 (28.0%). Furthermore, in response to items asking about the appropriateness of discussing OD in this setting, 71.5% of participants agreed with the statement, “A health workshop is a good place to discuss organ donation” and 73.1% of participants disagreed with the statement, “It is not appropriate to discuss organ donation at a health workshop.”
Discussion
This is the first study to examine attitudes regarding organ donation among participants in evidence-based chronic disease prevention/management programs. Most of the participants in these programs are over age 50 and have at least one chronic health condition including hypertension (61%) or diabetes (44%). This study aimed to test the psychometric properties of a previously developed scale with new items addressing older adults with chronic health conditions. Analyses identified three subscales: General Benefits, General Barriers, and Age/Health Barriers. Many participants reported believing being older adults and/or having a chronic health condition disqualified them from registering as organ donors. More education is needed to increase the number of these adults registered as organ donors.
In our study, the rate of positive donation status in age >45 years and with chronic disease was much lower than the Michigan Organ Donor Registry enrollment rate among all adult residents (37% vs. 62%). Similarly, 39% of respondents have a low intention to donate, and another 41% indicated medium intent. This reflects that many older adults who attend health workshops are not signed up to be donors and do not intend to sign up. Low intention to donate may be driven by misconceptions about the ability of older adults and those with chronic conditions to donate.
The surveys revealed that misconceptions about organ donation are present in this population. The mean scores (out of a 7-point scale) for Scales 1, 2, and 3 were 5.22, 5.85, and 5.05, respectively. Misconceptions about donation and low intention to donate are modifiable barriers. We believe that education tailored to this patient population, either at health workshops or other community events would change their attitudes towards registering for organ donation. This, in turn, will translate into improving registration rates for organ donation, over time, in this age group with chronic disease.
These findings indicate a need for increased intervention among older adults; a majority are eligible for many types of organ donation but nonetheless erroneously believe they are not candidates for donation. A health workshop, such as the CDSMP, DSMP, or DPP, appears to be a suitable venue for providing education to conduct such interventions. Over 70% of study participants indicated that a health workshop is an appropriate place for discussing organ donation. For the larger trial, Leave a Legacy of Life, the intervention included an hour long presentation given by a peer leader with a personal connection to organ donation. The presentation included the peer leader’s story, information to address common and age-related myths and barriers, tips for talking with your family, and how to sign up on the Michigan Organ Donor Registry; a brochure was provided for participants to sign up on site. This may also have implications for replication if the intervention is found to be effective. These evidencebased workshops are offered throughout the US; other communities may benefit from adding organ donation education to these programs as participants report openness to including them.
Female gender, white race, higher education level, and higher income level were identified as predictors/correlates to positive organ donation status. Age was not identified as a correlate, which is likely because 95% of the study group was over age 45 years. Our findings related to demographic variables were consistent with previous research. It is widely reported that those in Black/African American, Hispanic, or other minority communities report less positive attitudes towards organ donation and greater mistrust of the medical system [19-22]. Other studies have also reported that females have more positive attitudes towards organ donation [23], as well as those with higher education attainment and income [24]. Our research consortium’s past intervention trials among African American churches and Greek organizations utilized a peer or lay leader model, with a trusted member of the community sharing information about organ donation [25,26]. Utilizing a peer leader may help to alleviate distrust and increase enrollment in the donor registry.
Our study has several limitations. The sample was not randomly drawn so selection bias is present; we surveyed individuals who enrolled in CDSMP, DSMP, and DPP and persons could opt out. Individuals who self-enroll in a health management workshop may not be reflective of the general older adult population. Therefore, we lack generalizability. In addition, data was self-reported and we could not validate donor registry enrollment status. Furthermore, there was a significant difference at baseline in the intervention and the control groups with regards to their current donor status, with the intervention group having a higher base rate of registration (39% vs. 33%). The study was cross-sectional so a longitudinal study examining the association of attitudes and donation behaviors is warranted.
In conclusion, our study found that there are general barriers as well as age and health related barriers associated with low intent to donate in a specific group (age >45 years with one chronic condition and attended a health workshop). A tailored, educational intervention that addresses the barriers and misconceptions through health workshops or other community engagement may improve intent to register for organ donation and increase the organ donation rates among older adults with chronic conditions.
Acknowledgments-Funding Support
This project was supported by the HRSA of the U.S. Department of Health and Human Services (HHS) under grant number R39OT26992, Integrating Organ Donation Messages into Evidence-Based Programs. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
Conflict of Interests
None declared.
References
- Wynn JJ, Alexander CE (2011) Increasing organ donation and transplantation: the US experience over the past decade. Transpl Int 24: 324-332.
- Hart A, Smith JM, Skeans MA, Gustafson SK, Wilk AR, et al. (2018) OPTN/SRTR 2016 Annual Data Report: Kidney. Am J Transplant 18: 18-113.
- U.S. Department of Health and Human Services, Health Resources and Services Administration, Healthcare Systems Bureau (2013) 2012 National Survey of Organ Donation Attitudes and Behaviors. U.S. Department of Health and Human Services: Rockville, MD.
- Abecassis M, Bridges ND, Clancy CJ, Drew MA, Eldadah B, et al. (2012) Solid‐Organ Transplantation in Older Adults: Current Status and Future Research. Am J Transplant 12: 2608-2622.
- Downing K, Jones LL (2008) Designing an educational strategy for increasing organ donor registration among older adults. Prog Transplant 18: 290-296.
- Quick BL, Anker AE, Feeley TH, Morgan SE (2016) An examination of three theoretical models to explain the organ donation attitude-registration discrepancy among mature adults. Health Commun 31: 265-274.
- Cameron AM, Massie AB, Alexander CE, Stewart B, Montgomery RA, et al. (2013) Social media and organ donor registration: the Facebook effect. Am J Transplant 13: 2059-2065.
- Perrin A (2015) Social media usage. Pew research center.
- Goldberg DS, Halpern SD, Reese PP (2013) Deceased organ donation consent rates among racial and ethnic minorities and older potential donors. Crit Care Med 41: 496-505.
- Brown CV, Foulkrod KH, Dworaczyk S, Thompson K, Elliot E, et al. (2010) Barriers to obtaining family consent for potential organ donors. J Trauma Acute Care Surg 68: 447-451.
- Van Leiden HA, Jansen NE, Haase-Kromwijk BJ, Hoitsma AJ (2010) Higher refusal rates for organ donation among older potential donors in the Netherlands: impact of the donor register and relatives. Transplant 90: 677-682.
- https://www.giftoflifemichigan.org/about-donation/map-michigan-donors
- Resnicow K, Andrews AM, Zhang N, Chapman R, Beach D, et al. (2012) Development of a scale to measure African American attitudes toward organ donation. J Health Psychol 17: 389-398.
- Andrews AM, Zhang N, Buechley C, Chapman R, Guillen JL, et al. (2016) Organ Donation Attitudes and Practices among African Americans: An Adapted Measurement Instrument. J Health Care Poor Underserved 27: 1397-1410.
- Morgan SE, Stephenson MT, Harrison TR, Afifi WA, Long SD. (2008) Facts versus Feelings: How Rational Is the Decision to Become an Organ Donor? J Health Psychol 13: 644-658.
- Lorig KR, Sobel DS, Stewart AL, Brown Jr BW, Bandura A, et al. (1999) Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care 37: 5-14.
- Lorig K, Ritter PL, Villa FJ, Armas J (2009) Community-based peer-led diabetes self-management. The Diabetes Educator 35: 641-651.
- American Diabetes Association (2005) Impact of intensive lifestyle and metformin therapy on cardiovascular disease risk factors in the diabetes prevention program. Diabetes care 28: 888-894.
- Siminoff LA, Burant CJ, Ibrahim SA (2006) Racial disparities in preferences and perceptions regarding organ donation. J Gen Intern Med 21: 995-1000.
- Robinson DH, Klammer SMG, Perryman JP, Thompson NJ, Arriola KR (2014) Understanding African American's religious beliefs and organ donation intentions. J Relig Health 53: 1857-1872.
- Quick BL, LaVoie NR, Reynolds-Tylus T, Bosch D, Morgan SE (2016) Does Donor Status, Race, and Biological Sex Predict Organ Donor Registration Barriers? J Natl Med Assoc 108: 140-146.
- Moore SA, Myers O, Comfort D, Lu SW, Tawil I, et al. (2014) Effects of ethnicity on deceased organ donation in a minority-majority state. Crit Care Med 42: 1386-1391.
- Weber K, Martin M, Binkowski T, Cicchirillo V, Hogan S, et al. (2006) Gender and consent to organ donation. J social psychol 146: 247-249.
- Boulware LE, Ratner LE, Sosa JA, Cooper LA, LaVeist TA, et al. (2002) Determinants of willingness to donate living related and cadaveric organs: identifying opportunities for intervention. Transplant 73: 1683-1691.
- Andrews AM, Zhang N, Magee JC, Chapman R, Langford AT, et al. (2012) Increasing donor designation through black churches: results of a randomized trial. Prog Transplant 22: 161-167.
- Loughery C, Zhang N, Resnicow K, Chapman R, Magee JC, et al. (2017) Peer Leaders Increase Organ Donor Designation Among Members of Historically African American Fraternities and Sororities. Prog Transplant 27: 369-376.