Case Report, J Blood Res Hematol Dis Vol: 7 Issue: 4
Thromboelastrography in Boomslang Envenomation (Dispholidus typus)
Jonathan Chen* and Ryan Davids
Department of Anaesthesiology and Critical Care, Stellenbosch University, Stellenbosch, South Africa
*Corresponding Author: Jonathan Chen, Department of Anaesthesiology and Critical Care, Stellenbosch University, Stellenbosch, South Africa, Tel: +27 72 8683393; E-mail: chenjonathan123@hotmail.com
Received date: 13 July, 2022, Manuscript No. JBRHD-22-69203; Editor assigned date: 15 July, 2022, PreQC No. JBRHD-22-69203 (PQ); Reviewed date: 29 July, 2022, QC No. JBRHD-22-69203; Revised date: 04 October, 2022, Manuscript No. JBRHD-22-69203 (R); Published date: 11 October, 2022, DOI:10.4172/jbrhd.1000156.
Citation: Chen J, Davids R (2022) Thromboelastrography in Boomslang Envenomation (Dispholidus typus). J Blood Res Hematol Dis 7:4.
Abstract
A 33 years male presented with haemotoxic envenomation after being bitten by a boomslang (Dispholidus typus). The boomslang bite induces venom induced consumptive coagulopathy in which factors II, IX and X is activated. A procoagulant state is induced which may be evident within four hours but may be delayed by 72 hours.
Mr. M, presented with severe life threatening coagulopathy, his management and clinical improvement is demonstrated using thromboelastography in the form of ROTEM®. The case report demonstrates ROTEM findings after boomslang envenomation as well as the response to antivenom treatment. We highlight the importance of thromboelastography compared to traditional coagulation tests. We also reflect on the use of plasma derived blood products in the treatment of coagulopathy induced envenomation as opposed to antivenom therapy in correcting the coagulopathy.
Keywords
Snake bite; Coagulopathy; Envenomation; Boomslang
Introduction
The boomslang ('tree snake' in Afrikaans), Dispholidus typus, is one of few medically important venomous snakes of the family Colubridae. Boomslang envenomation is uncommonly reported and herpetologists often note the non-confrontational nature of the species. When approached, these snakes will commonly inflate their neck as part of a warning display.
Although many medically important snakes do contain venom that induce coagulopathy; manifestations of active bleeding are relatively uncommon such as found in boomslang. This is owed to its appreciable portions of venom metalloproteases resulting in a Venom Induced Consumptive Coagulopathy (VICC), physiologically explained by defibrinogenation [1].
The monovalent antivenom targeted at neutralizing boomslang venom is produced from equine serum. The equine immunologic products poses significant risk of anaphylaxis and risk benefit consideration should always be considered prior to administration [2].
Case Presentation
Mr. M, a healthy 33 years male with no medical or surgical history encountered a boomslang on his property. In an attempt to remove the snake Mr. M was bitten on his right forearm at 16 h00. He reported that the snake remained attached to his forearm for less than 30 seconds until he managed to forcefully pull it off and kill it. He did not seek immediate medical attention or do any first aid pertaining to the bite mark. The following morning (14 hrs later), Mr. M noticed a few concerning symptoms. Alarmed by the gum bleeding, macroscopic haematuria and ongoing slow bleed from the bite site on his forearm, Mr. M sought medical attention and brought along the snake for identification.
At the nearest hospital, his vitals are documented as BP 120/88, pulse 63, respiration rate 18, saturation 99% and haemoglobin 15 g/dl.
The hospital had no access to antivenom, the treating team concerned about the worsening coagulopathy arranged transport to the nearest academic hospital.
Upon arrival to the academic centre Mr. M was assessed as being clinically stable, all vital signs were within normal range and haemoglobin count of 9,8 g/dL. The poison centre identified the snake as boomslang also affirmed by resident herpetologist. Two fang marks were noted on his right forearm with blood oozing from these sites, to which gauze dressings were applied.
The initial assessment of M included blood tests (Complete blood count, chemistry and coagulation profile). It was noted that the clot activator serum separator specimen remained completely unclotted after four hours.
His attending doctor administered 0.5 ml tetanus toxoid intramuscularly into the right deltoid Figure 1. (It should be noted that this is contra-indicated in a patient with suspected coagulopathy).

Figure 1: Bruising from anti-tetanus toxoid intramuscular injection on right deltoid.
The patient continued to bleed from all puncture sites as well as his gums, with frank macroscopic haematuria. His coagulation profile was initially unrecordable but on repeat showed an INR of >10, PT 180 seconds and PTT >180 seconds. Platelets were not affected and always above 200 109/l (All results were laboratory instrumented tested).
Vital signs demonstrated Mr. M’s heart rate at 60 beats per minute, his blood pressure 123/77 and a respiratory rate of 16 breaths per minute.
The decision was taken to admit Mr. M into the intensive care unit prior to antivenom administration to mitigate, monitor and potentially manage the anaphylaxis risk (Figure 2).
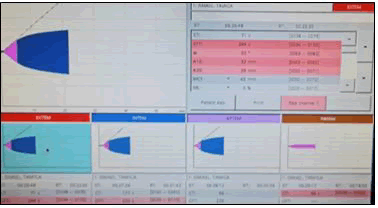
Figure 2: Antivenom administration to mitigate, monitor and potentially manage the anaphylaxis risk.
A baseline ROTEM® was performed prior to two vials (20 ml) of monovalent antivenom administration, which was infused over 30 minutes.
This monovalent anti-venom is manufactured from refined equine serum by South African vaccine producers.
Mr. M was subjected to haemodynamic monitoring during and after the antivenom administration. No clinical manifestation of hypersensitivity was noted. The patient received the antivenom 69 hours after injury.
Within the next 12 hours Mr M reported absence of gum bleeding and resolved haematuria. His coagulation profile was repeated, along with the ROTEM® (Figure 3.)
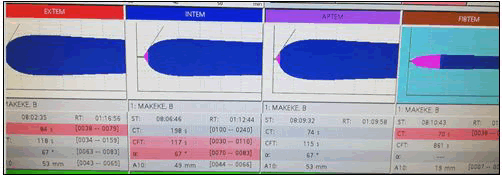
Figure 3: ROTEM® after anti-venom administration showed resolved coagulopathy.
Mr. M was discharged from the intensive care unit and no further complications were reported.
Discussion
The burden of snake bite emergencies is highly variable between countries [3]. Although a rare presentation the immediate management and treatment of envenomation remains essential care of any emergency unit.
Management based on a syndromic approach is often advocated. In the setting of haemotoxic envenomation the approach hinges on the correction of the venom induced consumptive coagulopathy, in which factors II, IX and X are activated. A procoagulant state is induced which may be evident within four hours of incident but may be delayed by 72 hours.
As with other causes of coagulopathy the instinctive management is to transfuse blood and blood products for symptomatic therapy.
This therapy has been attempted in many case reports on haemotoxic envenomation. The use of Fresh Frozen Plasma (FFP) and derived products utilized in the management of boomslang bites has been demonstrated to be largely futile. One such case by Krüger, administered blood and FFP as no antivenom was available; their patient demised due to uncontrolled haematemesis. Another case by Tambwe, administered only one vial of antivenom and five units of cryoprecipitate and still required another vial of antivenom to achieve normal coagulation values; indicating that the cryoprecipitate was ineffective at correcting the fibrinogen deficiency.
Reliance on blood and blood products as a means to correct VICC is not only ineffective in the case of the boomslang, it is potentially hazardous. Similar futility was demonstrated in haemotoxic envenomation induced by vipers (family Viperidae) [4-10]. Viper studies echo the sentiment that FFP and adjuncts are ineffective at reversing coagulopathy and may in itself pose unnecessary risk. It is important to note that studies supporting use of FFP in haemotoxic snake bites specifically state that FFP may be beneficial but only after antivenom administration and in the event that coagulopathy appears to be resolving [11,12].
Not with standing the anaphylactic risks, the remaining controversies around antivenom administration encircle timing and dosage of the agent. The timing of antivenom administration in this case was 69 hours after the injury. The effectiveness of antivenom from time of injury is not universally agreed upon; similarly the literature is saturated with reports of incorrect antivenom dosing, often reports of under-dosing. These controversies are mitigated with use of pointof- care testing as with ROTEM®. The degree of coagulopathy as well as the response to therapy is clearly demonstrated using thromboelastography.
A paucity of data exists relating to the use of thromboelastography in haemotoxic snake bites. Albeit available evidence points towards particular benefit in recognising coagulopathy prior to evident clinical signs [13-16]. This case highlights the use of thromboelastography in haemotoxin envenomation as a diagnostic, severity and treatment response tool. Further to this point the case serves to add to the body of literature reflecting the superiority of antivenom over conventional allogenic blood strategies to restore coagulation.
Conclusion
Monovalent antivenom is an efficient agent for the complete reversal of coagulopathy in boomslang envenomation, mitigating the use and need for additional blood or blood products.
The case further proves that thromboelastography is an effective tool for diagnosis, severity and treatment monitoring of haemotoxic envenomation. Highlighting the longer turnaround times and chance of unrecordable results of traditional coagulation studies.
References
- Debono J, Dobson J, Casewell NR, Romilio A, Li B, et al. (2017) Coagulating Colubrids: Evolutionary, Pathophysiological and Biodiscovery Implications of Venom Variations between Boomslang (Dispholidus typus) and Twig Snake (Thelotornis mossambicanus). Toxins 9:171.
- Tambwe MJ, Lalloo V, Engelbrecht A, Pelle P (2021) A case report of detecting subclinical coagulopathy in a patient with boomslang (Dipholidus typus) bite. S Afr Fam Pract 63:1-5.
- Krüger, Johannes H, Lemke FG (2019) Fatal Boomslang bite in the Northern Cape. Afr J Emerg Med 9:53-55.
- Nivy R, Aroch I, Bruchim Y (2020) Efficacy of specific antivenom and fresh frozen plasma in reversing Daboia palaestinae venom-induced hemostatic derangement. J Vet Emerg Crit Care (San Antonio) 30:396-404.
- Eddington JA, Wingert WA (1986) Timing of the administration of antivenom. Toxicon 24:421-423.
- Isbister GK, Jayamanne S, Mohamed F, Dawson AH, Maduwage K, et al. (2017) A randomized controlled trial of fresh frozen plasma for coagulopathy in Russell's viper (Daboia russelii) envenoming. J Thromb Haemost 15:645-654.
- Paul V, Prahlad KA, Earali J, Francis S, Lewis F (2003) Trial of heparin in viper bites. J Assoc Physicians India 51:163-166.
- Paul V, Pudoor A, Earali J, John B, Kumar CSA, et al. (2007) Trial of low molecular weight heparin in the treatment of viper bites. J Assoc Physicians India. 55:338-342.
[Googlescholar] [Indexed]
- Rathnayaka RMMKN, Ranathunga PEAN, Kularatne SAM (2020) Venom-induced consumption coagulopathy following hump-nosed pit viper envenoming in sri lanka: uncertain efficacy of fresh frozen plasma. Wilderness Environ Med 31:131-143.
[Crossref] [Googlescholar][Indexed]
- Kumara H, Seneviratne N, Jayaratne DS, Siribaddana S, Isbister GK, et al. (2019) Severe coagulopathy in Merrem's hump-nosed pit viper (Hypnale hypnale) envenoming unresponsive to fresh frozen plasma: A case report. Toxicon 163:19-22.
- Isbister GK, Buckley NA, Page CB, Scorgie FE, Lincz LF, et al. (2013) A randomized controlled trial of fresh frozen plasma for treating venom-induced consumption coagulopathy in cases of Australian snakebite (ASP-18). J Thromb Haemost 11:1310-1318.
[Crossref] [Googlescholar] [Indexed]
- Holla SK, Rao HA, Shenoy D, Boloor A, Boyanagari M (2018) The role of fresh frozen plasma in reducing the volume of anti-snake venom in snakebite envenomation. Trop Doct 48:89-93.
- Hadley GP, McGarr P, Mars M (1999) The role of thromboelastography in the management of children with snake-bite in southern Africa. Trans R Soc Trop Med Hyg 93:177-179.
[Crossref] [Googlescholar][Indexed]
- Rushton WF, Rivera JV, Brown J, Kurz MC, Arnold J (2021) Utilization of thromboelastograms in management of Crotalus adamanteus envenomation. Clin Toxicol (Phila). 59:256-259.
- Muller G, Wium C, Modler H, Veale D (2012) Snake bite in southern Africa: diagnosis and management. Contin Med Educ 30:362-381.
- Rodrigo C, Gnanathasan A (2020) Adjunct treatment in snakebite envenoming: A systematic review of randomised controlled trials. Trans R Soc Trop Med Hyg 114:847-857.
